Opening Sterile Surgical Instrument Containers
Main Text
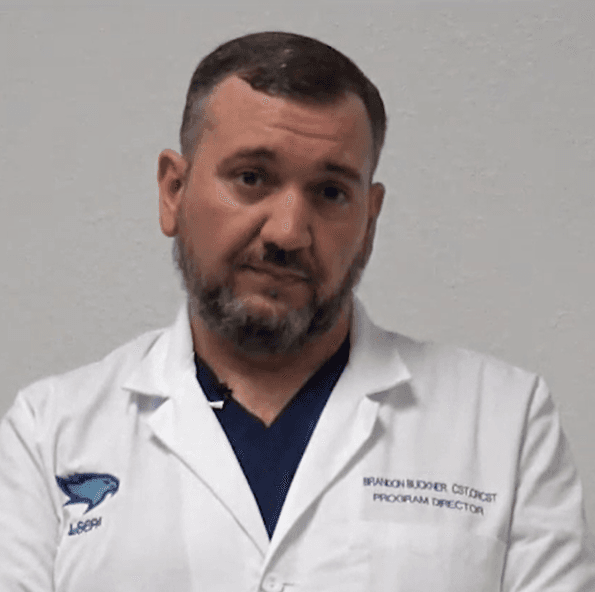
This video article demonstrates the proper handling and verification process for reusable rigid surgical instrument containers, using a laparoscopic set as an example. It highlights external sterility indicators, including a chemical indicator lock and Julian date sticker, and outlines step-by-step protocols for safe opening and inspection. Emphasis is placed on minimizing contamination risks through coordinated handling, filter integrity checks, and timing of sterile field setup. The tutorial underscores the importance of maintaining sterility to ensure operative safety and efficiency.
In contemporary healthcare settings, the need to balance efficiency, cost-effectiveness, and environmental responsibility has led to the widespread adoption of reusable containers for surgical instruments.1,2 This video demonstrates the advantages of employing reusable rigid containers for surgical instruments, using a laparoscopic set from Baptist Hospitals of Southeast Texas as a case study.
The external features of this container provide visual cues regarding the sterility of the enclosed instruments. A prominent feature of the container is the chemical indicator-based fluorescent orange lock, which serves as the primary mechanism for securing the instruments. Before opening the instrument set, healthcare professionals must visually inspect the lock to ensure that the seals remain intact and the chemical indicator has undergone the expected transition from white to black. This visible change in color serves as an indicator of successful sterilization.3 An additional feature of the container is a small "price tag" sticker affixed to the exterior. This sticker contains essential details about the autoclave used for sterilization, the load number, and the Julian date. The first two digits (YY) show the year of sterilization for the given item. The final three digits (DDD) show the day of the year, beginning with January 1 (001) and continuing with each day of the year in sequence. This information is important for monitoring and maintaining quality control standards.
The laparoscopic instrument set container is designed with locks on both sides, requiring a coordinated approach to prevent contamination during the opening process. Before opening the container, practitioners are advised to place a hand on either side of the locks. The locks are designed to break upon opening, with a potential for small pieces of plastic to be released in air. To mitigate the risk of contamination, practitioners are instructed to keep their hands over the locks as they simultaneously lift them. This opening approach minimizes the likelihood of plastic fragments becoming airborne. Upon breaking the locks, the container’s lid is lifted approximately 12 inches from the container. Simultaneously, practitioners rock back to create distance from the top of the set. This precautionary measure prevents the risk of fallout contamination.
After successfully lifting the lid, practitioners proceed with a detailed inspection, focusing on the chemical indicators of the filters located on the inner surface of the lid. To verify the set’s sterility, practitioners remove the cover from each filter and hold it up against a light source. This visual inspection aims to identify any potential issues such as holes and tears, which could indicate a breach in the filter’s integrity. Afterwards, the technician, having performed a hand scrub, approaches the container without touching it, to inspect the chemical indicator inside the container and confirms that the dark bar has completely traveled through the unsafe zone and has entered the safe zone.
Only then does the technician pick up the instrument set from the container and wait for the circulator to check the filters located at the bottom of the container in the same manner as discussed above. After confirming the integrity of the filters and the change in the color of the chemical indicators, the surgical technician places the instrument set on the sterile table. This meticulous process safeguards sterility and minimizes the risk of contamination in the surgical environment.
It is also worth mentioning that the establishment of sterile fields should ideally coincide with the timing of the procedure and should never be left unattended. The longer a sterile field is left open and exposed prior to the procedure, the greater the risk of contamination from airborne microbes.4
The successful outcome of surgical procedures relies on the accuracy and sterility of instruments, making the selection of instrument containers a critical aspect of OR protocols. This video provides a comprehensive tutorial on how to effectively utilize reusable rigid containers for surgical instruments.
Nothing to disclose.
Abstract added post-publication on 07/20/2025 to meet indexing and accessibility requirements. No changes were made to the article content.
Check out the rest of the series below:
References
- Keil M, Viere T, Helms K, Rogowski W. The impact of switching from single-use to reusable healthcare products: a transparency checklist and systematic review of life-cycle assessments. Eur J Public Health. 2023;33(1). doi:10.1093/eurpub/ckac174.
- Lam K, Gadi N, Acharya A, Winter Beatty J, Darzi A, Purkayastha S. Interventions for sustainable surgery: a systematic review. Int J Surg. 2023;109(5). doi:10.1097/JS9.0000000000000359.
- Centers for Disease Control and Prevention. Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008; Miscellaneous Inactivating Agents. CDC website. 2013;(May).
- Tennant K, Rivers CL. Sterile Technique. [Updated 2022 Sep 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
Cite this article
Buckner B, Romero C. Opening sterile surgical instrument containers. J Med Insight. 2024;2024(300.5). doi:10.24296/jomi/300.5.