Surgical Staplers
Main Text
This video provides an overview of the most commonly used surgical staplers, their categories, and intraoperative applications. It explains skin staplers, linear and circular staplers, clip appliers, and Endo GIA devices—emphasizing their construction, usage, and tissue-specific selection. Topics such as color-coded reloads, ergonomic handling, and single-use versus reusable designs are also addressed. The demonstration highlights key distinctions in stapling techniques across open and minimally invasive surgeries, underscoring the importance of proper device selection and surgical team familiarity for safe and efficient tissue approximation and anastomosis.
For nearly two centuries, surgeons have been using mechanical devices to approximate tissues and facilitate their healing process. Currently, surgical staplers are widely used and have become essential tools in surgery. Staples facilitate rapid wound closure, hence shortening the duration of the surgical procedure. In comparison to intradermal sutures, stapling is associated with better cosmetic outcomes.1 However, stapling results in more complications and prolongs hospital stay.2 3
Staplers are classified into five categories: circular, linear, linear cutting, ligating, and skin staplers. Furthermore, contemporary variations have emerged to accommodate minimally invasive surgery.4 Every category includes a variety of commercial models, each characterized by distinct features. With distinct names, color-coded features, and variations in length and tissue thickness, each stapler serves a specific purpose in the surgical setting. The distinct characteristics of various tissue types in the human body significantly influence the selection of staples. To achieve the best stapling results for any type of tissue, it is important to have a sufficient amount of time for the tissue to be compressed to allow elongation of the tissue being compressed, while preventing the possible risk of tearing.5
This video aims to provide a comprehensive overview of stapling instruments and their associated use. The skin staplers, presented first, are typically crafted from a titanium alloy with minimal reactivity with tissues. The sizing of skin staples, such as 35R for regular or 35W for wide, is crucial, and their deployment aims to approximate rather than strangulate the tissue. The intraoperative staplers are presented next. Inside the human body, clips are often used on structures such as the cystic duct and the homonymous artery during gallbladder surgery. Laparoscopically, clip appliers with digital readouts are employed. For gastrointestinal side-to-side anastomoses or partial lung and liver resections, surgeons may use stapling devices such as the gastrointestinal anastomosis (GIA) stapler, which lays down two rows of staples and cuts in between.
Linear staplers are reusable. There are linear staplers with and without cutting functions. The latter may have different surgical uses than those that have cutting properties (e.g. digestive tract reconstruction or incisions during liver resection). Linear staplers contain a handle at the opposite end of the jaw. The surgeon manipulates the jaw using its handle to apply staples to the incision. Every time the surgeon fires a staple, a row of staples is ejected and applied to the tissue. The reloads for linear staplers are color-coded based on their intended use: white for vascular, blue for regular tissue, and green for thicker tissues.
The end-to-end anastomosis (EEA) circular stapler serves specific purposes such as end-to-end anastomoses. Unlike reusable staplers, the EEA stapler is a one-time-use item and is discarded after use. The stapler joins two hollow organs, creating a stapled anastomosis. For endoscopic procedures, Endo GIA staplers provide versatility. They are available in various lengths, and their disposable units are color-coded as well. The staplers allow surgeons to manipulate and fire the device through trocars, being incredibly useful in the context of minimally invasive surgery (MIS).
Surgical staplers are a wide range of instruments that have distinct uses in surgical practice. From skin closure to gastrointestinal anastomosis, each stapler is designed to meet the unique demands of a given surgical intervention. The operative staff should understand the features and uses of staplers to effectively handle the complexity of these devices.
Nothing to disclose.
Abstract added post-publication on 07/18/2025 to meet indexing and accessibility requirements. No changes were made to the article content.
Check out the rest of the series below:
References
- Ku D, Koo DH, Bae DS. A prospective randomized control study comparing the effects of dermal staples and intradermal sutures on postoperative scarring after thyroidectomy. J Surg Res. 2020;256. doi:10.1016/j.jss.2020.06.052.
- Mackeen AD, Sullivan MV, Schuster M, Berghella V. Suture compared with staples for skin closure after Cesarean delivery: a systematic review and meta-analysis. Obs Gyn. 2022;140(2):293–303. doi:10.1097/AOG.0000000000004872.
-
Zhao E, Tarkin IS, Moloney GB. Subcuticular barbed suture and skin glue wound closure decreases reoperation and length of stay in geriatric hip fractures when compared with staples. J Am Acad Orthop Surg Glob Res Rev. 2021 Oct 4;5(10):e21.00205. doi:10.5435/JAAOSGlobal-D-21-00205.
- McGuire J, Wright IC, Leverment JN. Surgical staplers: a review. J R Coll Surg Edinb. 1997;42(1).
- Chekan E, Whelan RL. Surgical stapling device–tissue interactions: what surgeons need to know to improve patient outcomes. Med Dev: Evid Res. 2014;7. doi:10.2147/MDER.S67338.
Cite this article
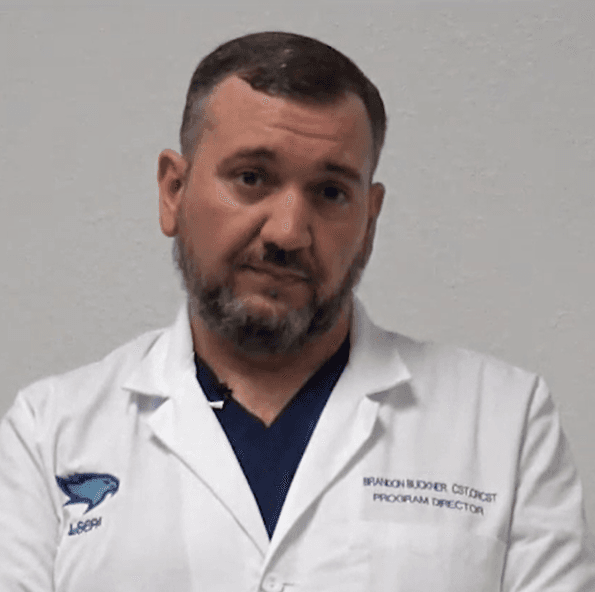
Buckner B. Surgical staplers. J Med Insight. 2024;2024(300.3). doi:10.24296/jomi/300.3.