Arthroscopic Bankart Repair for Anterior Shoulder Instability Using a Posterolateral Portal
Main Text
Table of Contents
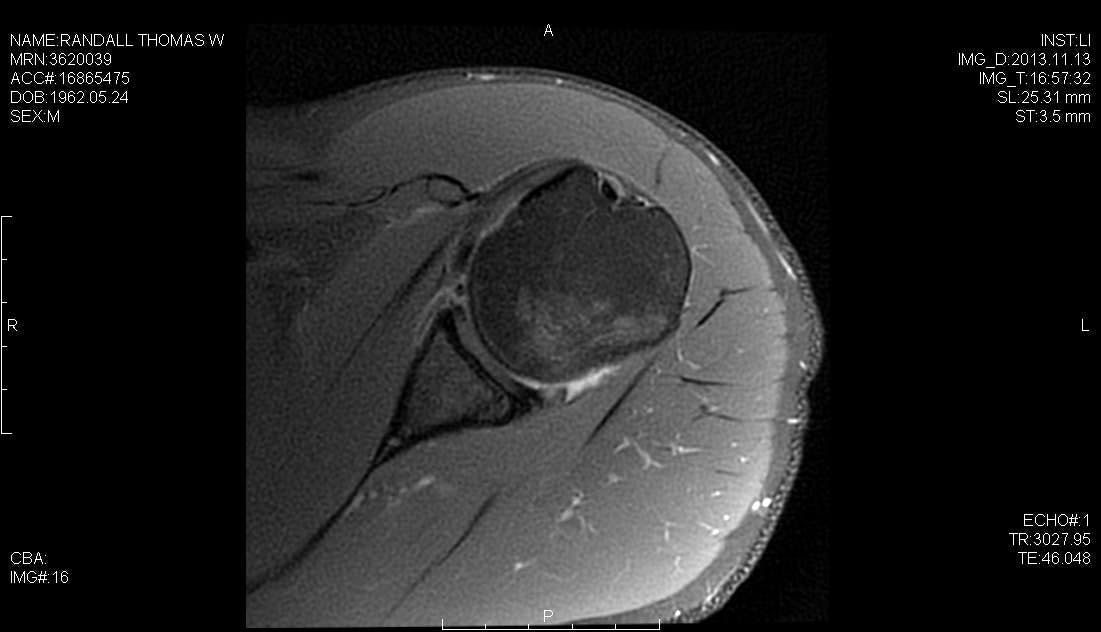
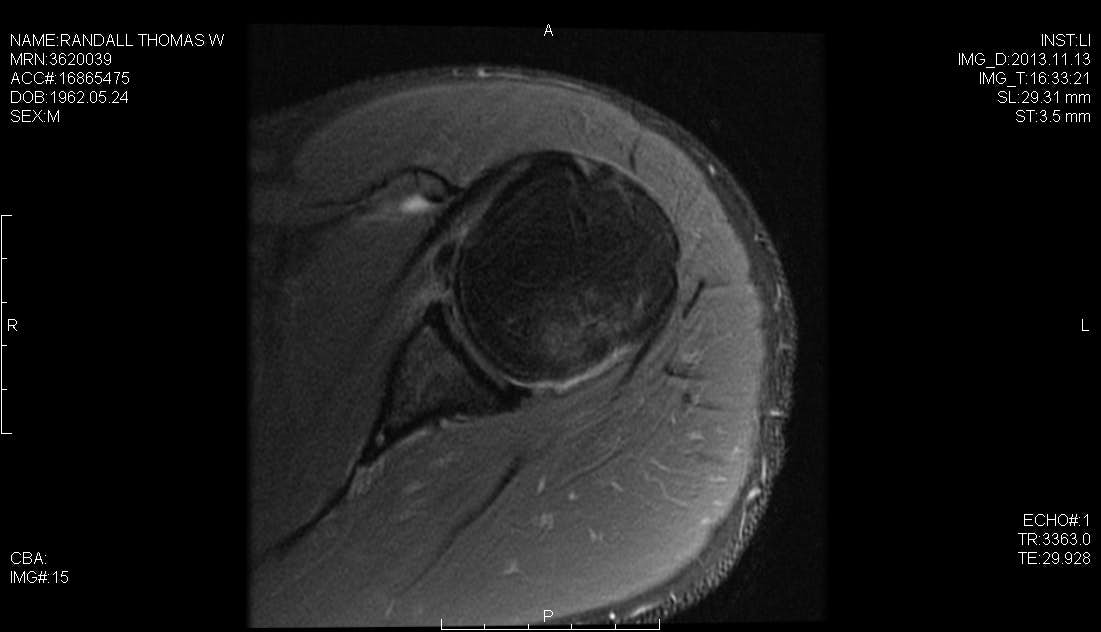
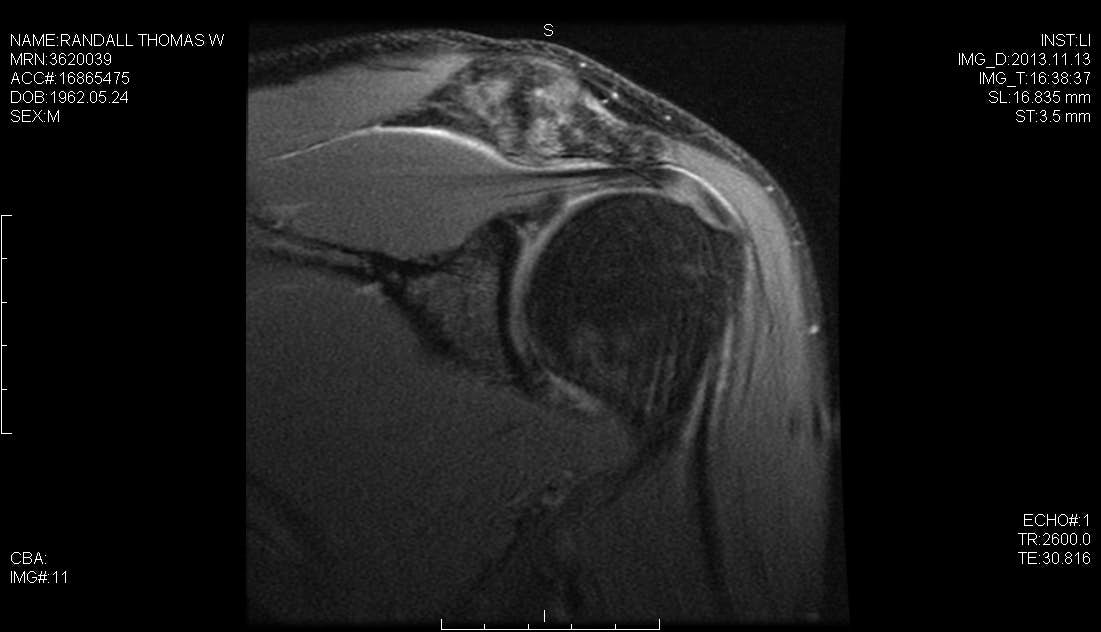
A successful surgical outcome for patients with shoulder instability requires a complete preoperative evaluation, a thorough diagnostic arthroscopy to evaluate for concomitant co-pathology, and an effective postoperative therapy program tailored to the repair strategy. In addition to the Bankart lesion, the surgeon must be aware of other co-pathologies such as the HAGL lesion, the ALPSA lesion and SLAP tears, all of which may occur in concert with capsular pathology and which present as potential barriers to a successful outcome. We have previously described the use of a posterolateral arthroscopic portal, 4 cm lateral to the posterolateral corner of the acromion. This portal simplifies and improves anchor placement, trajectory, and anatomic capsulolabral repair of the inferior glenoid. In this case, we perform a hybrid repair using the posterolateral portal to place the first suture anchor at the 6 o’clock position on the glenoid and the mid-glenoid portal to place two labral tape knotless anchors.
Obtain a history which includes past injury, trauma, and/or repetitive motions.- Has the patient dislocated? If so, how many times? What was the mechanism? How strong was the force required to dislocate?
- What limitations in activity have occurred? Is pain or instability present at rest? Does it interfere with sleep?
- What prior treatments, if any, has the patient already tried (i.e. physical therapy, rest, anti-inflammatory medication) and to what degree did these help?
- Palpate the shoulder for tenderness and document range of motion compared to the contralateral extremity. Differences between active and passive motion may indicate pain or capsular contracture.
- Test for impingement to determine whether rotator cuff tendinitis is present. If weakness is present during strength testing, it may be from deconditioning or from underlying rotator cuff or deltoid pathology.
- Tests for anterior instability
- Apprehension sign - performed with patient supine and the arm forward flexed 90 degrees and the elbow flexed 90 degrees. The patient exhibits apprehension when an anterior force is applied to the shoulder
- Relocation sign - the patient’s apprehension decreases when a posterior, supporting force is applied to the shoulder
- Sulcus sign - an inferior force is applied to the shoulder with the patient standing, arm at their side. Appearance of a depression below the acromion indicates a positive sulcus sign
- Recurrent instability
- Stiffness
- Infection
- Neurovascular injury
- Spectrum MVP suture passer ConMed Linvatec, Largo, FL
- 3.0mm Suture Tak Anchors, Arthrex, Naples, FL
- 2.9mm PEEK Knotless Labral Tape Anchor, Arthrex, Naples, FL
- 0 PDS Sutures, Ethicon, Somerville, NJ
Citations
- Seroyer ST, Nho SJ, Provencher MT, Romeo AA. Four-quadrant approach to capsulolabral repair: an arthroscopic road map to the glenoid. Arthroscopy. 2010;26(4):555-562. doi:10.1016/j.arthro.2009.09.019.
- Nord KD, Brady PC, Yazdani RS, Burkhart SS. The anatomy and function of the low posterolateral portal in addressing posterior labral pathology. Arthroscopy. 2007;23(9):999-1005. doi:10.1016/j.arthro.2007.04.011.
- Davidson PA, Rivenburgh DW. The 7-o'clock posteroinferior portal for shoulder arthroscopy. Am J Sports Med. 2002;30(5):693-696. doi:h10.1177/03635465020300051101.
- Difelice GS, Williams RJ III, Cohen MS, Warren RF. The accessory posterior portal for shoulder arthroscopy: description of technique and cadaveric study. Arthroscopy. 2001;17(8):888-891. doi:10.1016/S0749-8063(01)90015-5.
- Parameswaran AD, Provencher MT, Bach BR Jr, Verma N, Romeo AA. Humeral avulsion of the glenohumeral ligament: injury pattern and arthroscopic repair techniques. Orthopedics. 2008;31(8):773-779. doi:10.3928/01477447-20080801-21.
- Bradley JP, Tejwani SG. Arthroscopic management of posterior instability. Orthop Clin North Am. 2010;41(3):339-356. doi:10.1016/j.ocl.2010.02.002.
- Baker CL III, Romeo AA. Combined arthroscopic repair of a type IV SLAP tear and Bankart lesion. Arthroscopy. 2009;25(9):1045-1050. doi:10.1016/j.arthro.2009.04.075.
- Archetti Netto NA, Tamaoki MJS, Lenza M, et al. Treatment of Bankart lesions in traumatic anterior instability of the shoulder: a randomized controlled trial comparing arthroscopy and open techniques. Arthroscopy. 2012;28(7):900-908. doi:10.1016/j.arthro.2011.11.032.
- Waterman BR, Burns TC, McCriskin B, Kilcoyne K, Cameron KL, Owens BD. Outcomes after Bankart repair in a military population: predictors for surgical revision and long-term disability. Arthroscopy. 2014;30(2):172-177. doi:10.1016/j.arthro.2013.11.004.
Cite this article
Provencher M. Arthroscopic Bankart repair for anterior shoulder instability using a posterolateral portal. J Med Insight. 2014;2014(5). doi:10.24296/jomi/5.