Femoral Resurfacing with an Osteochondral Allograft for Osteochondritis Dissecans
Main Text
Table of Contents
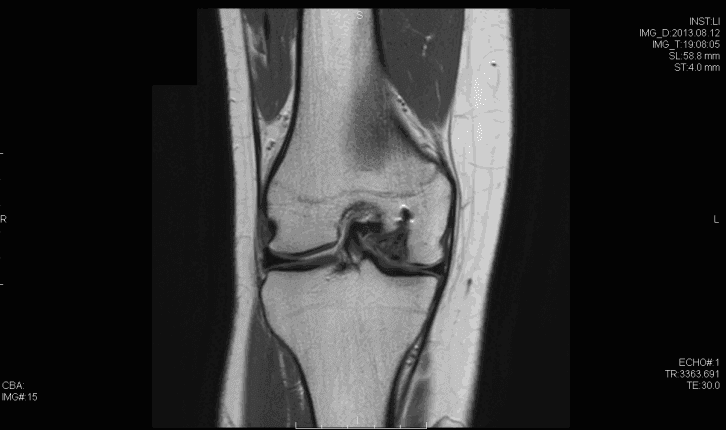
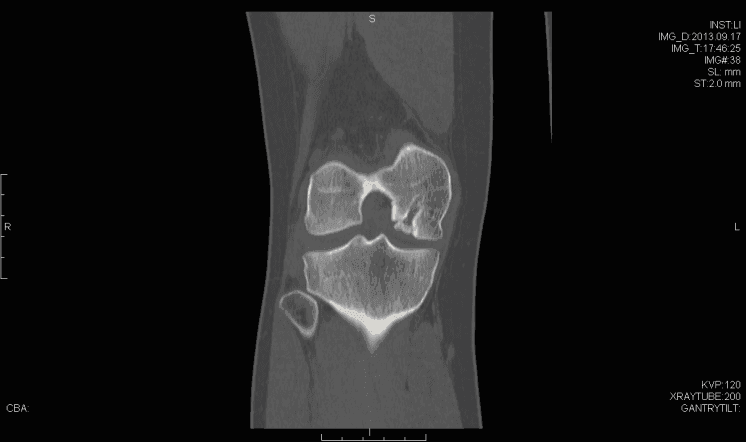
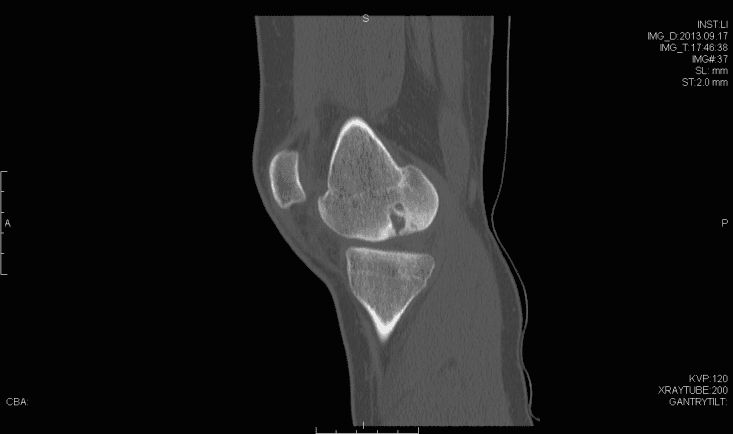
Osteochondritis dissecans (OCD) of the knee has multiple possible etiologies. Among these are repetitive microtrauma, disruption of normal endochondral ossification, as well genetic factors. The male to female ratio is approximately 4:1 in the United States and has been found to have the highest incidence in the African American population. Diagnosis is usually made by physical examination in association with radiographs (flexion notch view) and magnetic resonance imaging. Lesions are usually found on the lateral aspect of the medial femoral condyle. Arthroscopy continues to be the gold standard for assessing the stability of OCD lesions. Many unstable lesions may be treated with stabilization, and cartilage restoration may provide benefit; however long term data is still limited.
A history of the patient's knee problems should include the following questions:- Has there been any injury in the past? Any previous surgical treatment?
- What are the activities that the patient would like to return to?
- What limitations in activity, if any, have occurred as a result of the knee pain?
- Is pain or instability present at rest? Does it interfere with sleep?
- Has the patient had conservative treatments including physical therapy, rest, anti-inflammatory medication. If so, to what degree did these help?
- Aching, activity-related anterior knee pain,
- Antalgic gait,
- Effusion (only in unstable lesions)
- Mechanical symptoms (also only in unstable lesions)
- Softened area of intact cartilage
- Partial cartilage discontinuity, stable on probing
- Complete discontinuity, "dead in-situ"
- Dislocated fragment
- Small signal change, no clear margins
- OCD fragment with clear margins without fluid between fragment and bone
- Fluid partially visible between fragment and bone
- Fluid completely surrounds fragment
- Fragment displaced
Citations
- Mubarak SJ, Carroll NC. Juvenile osteochondritis dissecans of the knee: etiology. Clin Orthop Relat Res. 1981;157:200-211. https://journals.lww.com/clinorthop/Citation/1981/06000/Juvenile_Osteochondritis_Dissecans_of_the_Knee_.33.aspx.
- Robertson WBS, Kelly BT, Green DW. Osteochondritis dissecans of the knee in children. Curr Opin Pediatr. 2003;15(1):38-44. doi:10.1097/00008480-200302000-00007.
- Wall EJ, Vourazeris J, Myer GD, et al. The healing potential of stable juvenile osteochondritis dissecans knee lesions. J Bone Joint Surg Am. 2008;90(12):2655-2664. doi:10.2106/JBJS.G.01103.
- Kocher MS, Micheli LJ, Yaniv M, Zurakowski D, Ames A, Adrignolo AA. Functional and radiographic outcome of juvenile osteochondritis dissecans of the knee treated with transarticular arthroscopic drilling. Am J Sports Med. 2001;29(5):562-566. doi:10.1177/03635465010290050701.
- Adachi N, Deie M, Nakamae A, Ishikawa M, Motoyama M, Ochi M. Functional and radiographic outcome of stable juvenile osteochondritis dissecans of the knee treated with retroarticular drilling without bone grafting. Arthroscopy. 2009;25(2):145-152. doi:10.1016/j.arthro.2008.09.008.
- Kocher MS, Czarnecki JJ, Andersen JS, Micheli LJ. Internal fixation of juvenile osteochondritis dissecans lesions of the knee. Am J Sports Med. 2007;35(5):712-718. doi:10.1177/0363546506296608.
- Miura K, Ishibashi Y, Tsuda E, Sato H, Toh S. Results of arthroscopic fixation of osteochondritis dissecans lesion of the knee with cylindrical autogenous osteochondral plugs. Am J Sports Med. 2007;35(2):216-222. doi:10.1177/0363546506294360.
- Emmerson BC, Görtz S, Jamali AA, Chung C, Amiel D, Bugbee WD. Fresh osteochondral allografting in the treatment of osteochondritis dissecans of the femoral condyle. Am J Sports Med. 2007;35(6):907-914. doi:10.1177/0363546507299932.
- Gudas R, Simonaityte R, Cekanauskas E, Tamosiūnas R. A prospective, randomized clinical study of osteochondral autologous transplantation versus microfracture for the treatment of osteochondritis dissecans in the knee joint in children. J Pediatr Orthop. 2009;29(7):741-748. doi:10.1097/BPO.0b013e3181b8f6c7.
Cite this article
Provencher M. Femoral resurfacing with an osteochondral allograft for osteochondritis dissecans. J Med Insight. 2014;2014(4). doi:10.24296/jomi/4.