Transperitoneal Laparoscopic Right Adrenalectomy for Cortical Adenoma
Main Text
Table of Contents
Primary hyperaldosteronism, or Conn's syndrome, is a disease in which one or both adrenal glands produce excess amounts of aldosterone, leading to hypertension and hypokalemia. Common conditions resulting in this disorder include adenoma of the adrenal gland or hyperplasia of both adrenal glands. In rare cases, it is caused by malignant growth in the adrenal cortex or familial hyperaldosteronism. High blood pressure may cause headaches or blurred vision. Low potassium may cause fatigue, muscle cramps, muscle weakness, numbness, or temporary paralysis.
Primary hyperaldosteronism is diagnosed by measuring serum levels of aldosterone, renin, and potassium. Patients classically have high aldosterone levels, suppressed renin levels, and low potassium levels. Once the diagnosis is established, the localization of the source is performed using imaging studies. Adrenal vein sampling is also performed to determine more precisely and directly the side that is producing excess aldosterone.
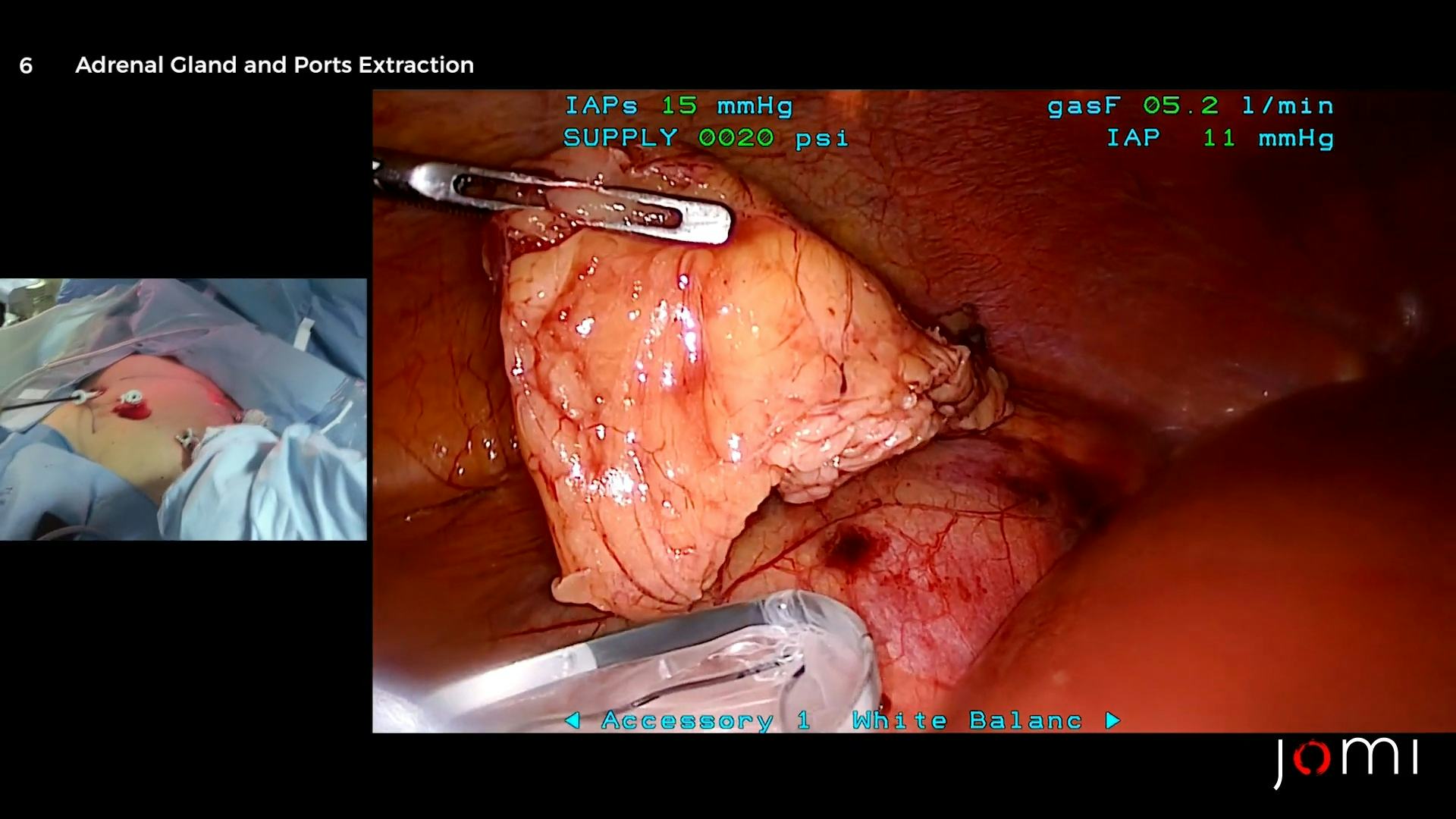
Primary hyperaldosteronism caused by an adrenal gland tumor is treated with adrenalectomy. Approximately 95% of patients will notice a significant improvement in their hypertension after successful surgery. Here, we present the case of a 58-year-old female with hypokalemia and long-standing hypertension refractory to medical treatment. Her blood tests showed high aldosterone levels and low renin levels, confirming the diagnosis of hyperaldosteronism. On CT scan, an adrenal nodule was noted on both sides. Adrenal vein sampling identified the right adrenal nodule as the cause. Laparoscopic access was gained, the adrenal gland was dissected and exposed, the adrenal vein ligated, and the adrenal gland was removed.
Primary aldosteronism was first described by Jerome Conn in 1956.1 The syndrome that bears Dr. Conn’s name is characterized by hypokalemia and hypertension, both of which are relatively refractory to medical management. Primary aldosteronism is a common, though underdiagnosed cause of secondary hypertension. Between 1–10% of patients with hypertension are thought to have underlying primary hyperaldosteronism.2
The most common causes of primary aldosteronism are primary aldosterone-producing tumors or hyperplasia of the zona glomerulosa of the adrenal gland.3
For patients with medication-resistant hypertension, a workup for Conn’s syndrome is indicated. If a unilateral tumor is identified as the source of the excess aldosterone, surgery to remove the tumor is indicated.
The patient is a 58-year-old female with long-standing hypertension. She had been treated with three medications with no satisfactory relief of her hypertension. Her laboratory examinations were notable for long-term hypokalemia, with her lowest recorded value being 2.3 mmol/L (normal range 3.6–5.2 mmol/L).
Her serum aldosterone and plasma renin activity (PRA) were measured to determine her aldosterone-to-renin ratio (ARR). Her serum aldosterone was 24 ng/dl, and her PRA was 0.6 ng/ml/h, giving an ARR of 40 (range of normal < 30 ng/mL/h).
After the CT scan showed bilateral adrenal lesions, adrenal vein sampling was performed to measure aldosterone and cortisol levels, and to determine their ratio using the inferior vena cava as the control (Table 1).4 The aldosterone levels in the right and left renal veins were 3,800 ng/dl and 78 ng/dl, respectively. The control value from the inferior vena cava was 66 ng/dl. Based on these values, including cortisol measurements, the calculated aldosterone/cortisol ratio of right vs left was 13.75. Any ratio over 4 is considered a positive finding. Taken together, the laboratory findings suggest that the right adrenal gland was the source of the excess aldosterone.
Table 1. Adrenal Vein Sampling
.png&w=1920&q=70)
*RT A:C ratio / LT A:C ratio > 4, suggesting that the right adrenal gland was the source of excess aldosterone.
Primary aldosteronism is not characterized by any particular sign on a physical exam. Nevertheless, long-standing hypertension may lead to left ventricular hypertrophy that may generate an S4 sound on auscultation. Other nonspecific signs include carotid bruits, muscular weakness, and mental status changes associated with hypertensive encephalopathy.3
An abdominal CT revealed a 2.6-cm lesion in the right adrenal gland and a 1.3-cm lesion in the left adrenal gland (Figure 1).
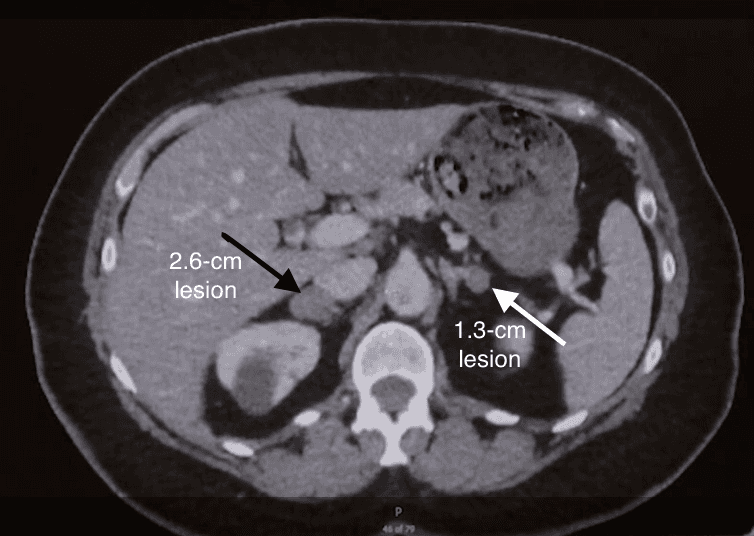
Figure 1. Abdominal CT
Noncontrast abdominal CT revealing a 2.6-cm lesion consistent with a right adrenal mass (black arrow), and a 1.3-cm lesion consistent with a left adrenal mass (white arrow).
Left untreated, the course of primary hyperaldosteronism is characterized by sequelae of hypokalemia and chronic hypertension. Muscle weakness and elevated serum creatine kinase levels secondary to hypokalemia have been reported as a presenting symptom and sign.5 Chronic hypertension places patients at greater risks of major adverse cardiac events, including atrial fibrillation, myocardial infarction, and stroke.3
Laparoscopic resection of unilateral adrenal tumors is the treatment of choice for Conn’s syndrome.6 However, some patients will be managed successfully with antihypertensive medications. Surgery is generally contraindicated in patients with bilateral disease; such patients are best managed medically with antihypertensive agents, including mineralocorticoid antagonists. The surgical approaches are primarily laparoscopic or retroperitoneoscopic.7
The goals of treatment are to reverse the patient’s hypokalemia and hypertension. The procedure reverses hypokalemia in virtually 100% of cases. However, patients are able to discontinue antihypertensive medications in only 35% of cases, though the degree of hypertension generally diminishes.8
Unilateral adrenalectomy is most effective when the disease is unilateral. Patients with bilateral hyperplasia or bilateral aldosterone-producing tumors (very rare) are generally not candidates for surgery and should be treated medically with blood pressure-lowering medications and aldosterone-blocking agents such as spironolactone.
Using a laparoscopic approach, we removed a 2.5-cm cortical adenoma from a 58-year-old woman with primary aldosteronism. One feature of this case worth noting is that the patient had evidence of bilateral tumors on CT; however, adrenal vein sampling suggested that the right-sided tumor was the source of her excess aldosterone.
We now, generally, send patients home the day of surgery (outpatient), provided they have no significant comorbidities. They are advised to continue to monitor their blood pressure at least twice per day and to take their blood pressure medications as prescribed (we usually cut down significantly on the number of agents and dosing). After discharge, we follow up closely with telephone calls later the same day and the following day.
This patient was discharged on only her beta-blocker. In the follow-up, we monitored her blood pressure and potassium levels. The goal with this patient was to wean her eventually off of all blood pressure medications.
- Endo Paddle
- Endo Catch Bag
None.
The patient referred to in this video article has given their informed consent to be filmed and is aware that information and images will be published online.
Citations
- Conn JW, Louis LH. Primary aldosteronism, a new clinical entity. Ann Intern Med. 1956;44(1):1-15. doi:10.7326/0003-4819-44-1-1.
- Piaditis G, Markou A, Papanastasiou L, Androulakis II, Kaltsas G. Progress in aldosteronism: a review of the prevalence of primary aldosteronism in pre-hypertension and hypertension. Eur J Endocrinol. 2015;172:R191-203. doi:10.1530/EJE-14-0537.
- Cobb A, Aeddula NR. Primary Hyperaldosteronism. [Updated 2019 Apr 21]. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539779/?report=classic.
- Deipolyi A, Bailin A, Wicky S, Alansari S, Oklu R. Adrenal vein sampling for Conn’s syndrome: diagnosis and clinical outcomes. Diagnostics. 2015;5(2):254-71. doi:10.3390/diagnostics5020254.
- Olt S, Yaylaci S, Tatli L, Gunduz Y, Garip T, Tamer A. Hypokalemia-induced myopathy and massive creatine kinase elevation as first manifestation of Conn's syndrome. Niger Med J. 2013;54(4):283. doi:10.4103/0300-1652.119658.
- Kim K, Kim JK, Lee CR, et al. Surgical outcomes of laparoscopic adrenalectomy for primary hyperaldosteronism: 20 years of experience in a single institution. Ann Surg Treat Res. 2019;96(5):223-9. doi:10.4174/astr.2019.96.5.223.
- Wierdak M, Sokołowski G, Natkaniec M, et al. Short- and long-term results of laparoscopic adrenalectomy for Conn’s syndrome. Wideochir Inne Tech Maloinwazyjne. 2018 Sep;13(3):292. doi:10.5114/wiitm.2018.74833.
- Parthasarathy HK, Ménard J, White WB, et al. A double-blind, randomized study comparing the antihypertensive effect of eplerenone and spironolactone in patients with hypertension and evidence of primary aldosteronism. J Hypertens. 2011 May;29(5):980-90. doi:10.1097/HJH.0b013e3283455ca5.
Cite this article
Cohen S, Hodin R. Transperitoneal laparoscopic right adrenalectomy for cortical adenoma. J Med Insight. 2023;2023(240). doi:10.24296/jomi/240.