Microsurgical Technique for 1mm Vessel End to End Anastomosis
Main Text
Table of Contents
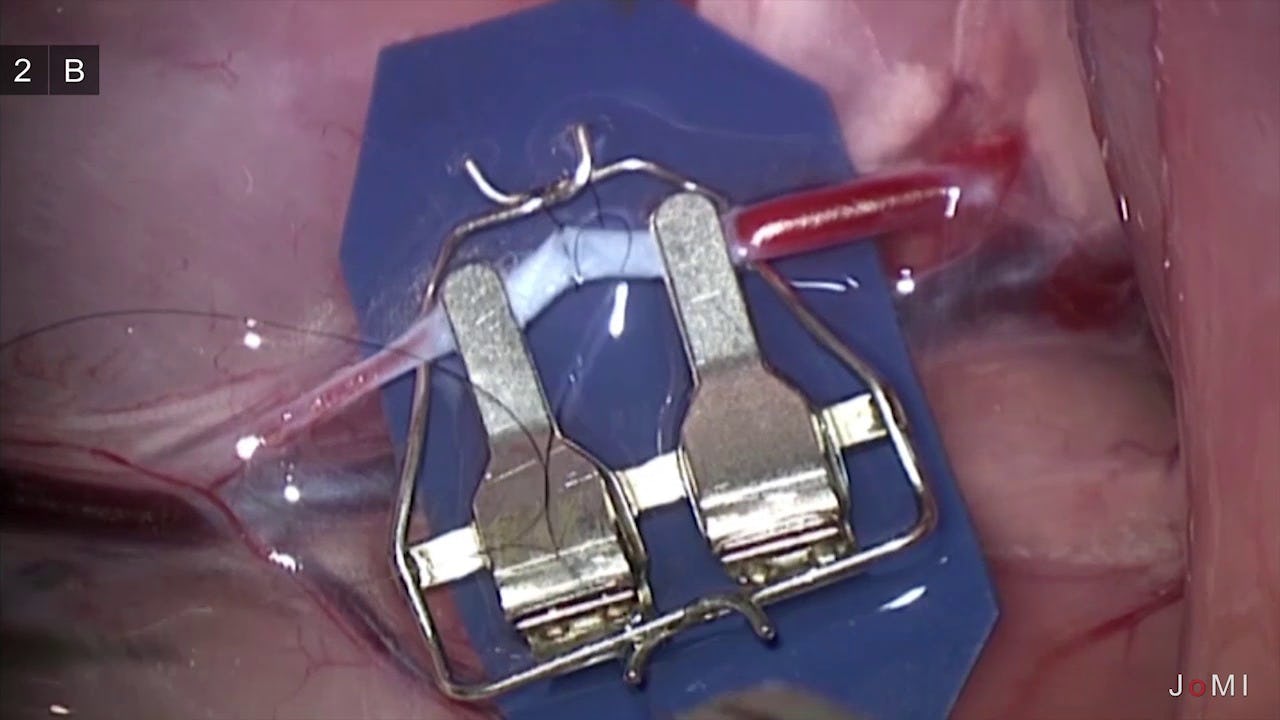
This article describes the technique of performing an end-to-end arterial anastomosis on a 1mm diameter rat femoral artery. Microsurgery anastomosis is a technique required for free flap transfers, transplant surgery and other surgical applications. This video article shows the microsurgical anastomosis technique in detail, covering aspects that are difficult to grasp without direct visualization. The laboratory environment is ideal tor practicing the delicate and meticulous maneuvers of microsurgery and for becoming familiar with the microscope and specialized tools involved. We hope this article will familiarize the prospective trainee prior to taking courses at our laboratory.
- Carl Zeiss OPMI MC surgical stereo microscope
- Optronics Video system
- Standard Microsurgery instruments
- 10-0 nylon sutures
The development of microsurgical anastomosis has allowed complex reconstructive surgical procedures including free tissue transfer grafts to cover large tissue defects, replantation of limbs, fingers, toes, and the revascularization of poorly perfused organs. The closure or coverage of large defects after trauma or tumor resection often requires free tissue transfer grafts and numerous anastomoses. Microsurgical techniques may also be used as a new approach to achieve lymphatic drainage in cases of lymphedema.
Dr. Jules Jacobson at the University of Vermont first described the use of a microscope to anastomose vessels as small as 1.4 mm in 1960. In 1963, hand surgeons at the University of Louisville, Dr. Harold Kleinert and Dr. Mort Kasdan, performed the first revascularization of a partial digital amputation. In 1964 Dr. Harry J. Buncke, working out of a lab created in his garage, successfully replanted a rabbit ear, anastomosing blood vessels 1 mm in diameter. Modern microsurgical techniques are now fundamental tools of plastic surgery, allowing soft tissue coverage and restoration of function after trauma or oncologic resections.
After the anastomosis is made, it must heal and mature if it is to survive. Formation of a platelet plug is the first step in a sequence of events towards healing and maturation of a fresh anastomosis. With injury to the intima, exposed collagen triggers platelet adhesion and aggregation. This in turn activates fibrinogen, which adheres to platelets and acts to link platelets together to form a platelet plug. Fibrinogen is then converted to fibrin which strengthens the platelet plug. If the vessel walls are not damaged and the anastomosis is secure, the platelet plug disappears over the first 3 to 5 days and by day 5 the pseudointima is present. One to two weeks later the anastomotic site is covered with new endothelium.
However, if there is too much damage to the endothelium, platelet aggregation continues and after reaching a certain critical mass it will trigger a cascade of events leading to thrombus formation in the vessel. The critical period of thrombus formation in the anastomosis is the first 3-5 days of healing. If a thrombus forms and is not cleared, the anastomosis will fail.
- Vessels are prepared by debriding any areas damaged by trauma
- Remove any intravascular clots and debris and irrigate with heparinized saline
- For end to end anastomosis as is shown in this article, the ends of the two vessels should be approximately the same in size
- Vessel side branches are examined and ligated to prevent hematoma formation
- Avoid vessel tension, kinking, and twisting. If tension is excessive it is preferable to perform a vein grafting
- Standard sutures are simple, interrupted, and full-thickness. These are the standard to which all new anastomotic techniques are compared.
- After flow is established, bathe the anastomotic sites in warm irrigation and lidocaine or papaverine to relieve vasospasm
- Examine anastomoses at the end of the procedure and perform the vascular strip test to check flow. To perform the strip test:
- Gently occlude the vessel distal to the anastomosis with a microforceps and "strip" the vessel with another microforceps in the direction of flow distally from the anastomosis
- Brisk blood flow should then be observed to return across the anastomosis with a good distal pulsation when the proximal microforceps are released
The author has no financial relationship with the equipment companies mentioned in this article.
This procedure was performed according to protocols that have been reviewed and approved of by IUCUC at Columbia University.
Citations
- Leung CC, Ghanem AM, Tos P, Ionac M, Froschauer S, Myers SR. Towards a global understanding and standardisation of education and training in microsurgery. Arch Plast Surg. 2013;40(4):304-311. doi:10.5999/aps.2013.40.4.304.
- Myers SR, Froschauer S, Akelina Y, Tos P, Kim JT, Ghanem AM. Microsurgery training for the twenty-first century. Arch Plast Surg. 2013;40(4):302-303. doi:10.5999/aps.2013.40.4.302.
- Martins PN, Montero EF. Basic microsurgery training. Comments and proposal. Acta Cir Bras. 2007;22(1):79-81. doi:10.1590/S0102-86502007000100014.
- Raine T. Microvascular techniques. In: Jurkiewicz MJ, Krizek TJ, Mathes SJ, Ariyan S, eds. Plastic Surgery: Principles and Practice. St. Louis, MO: Mosby; 1990:1573-1591.
- Sanders WE. Principles of microvascular surgery. In: Green DP, ed. Operative Hand Surgery. 3rd ed. New York, NY: Churchill Livingstone; 1993:1039-1083.
- Serafin D. Atlas of Microsurgical Composite Tissue Transplantation. Philadelphia, PA: Saunders; 1996.
- Shenaq SM, Sharma SK. Principles of microvascular surgery. In: Aston SJ, Beasley RW, Thorne CHM, eds. Grabb and Smith's Plastic Surgery. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 1997:73-77.
- Hayhurst JW, O'Brien BM. An experimental study of microvascular technique, patency rates and related factors. Br J Plast Surg. 1975;28(2):128-132. doi:10.1016/S0007-1226(75)90175-7.
- Moran SL, Illig KA, Green RM, Serletti JM. Free-tissue transfer in patients with peripheral vascular disease: a 10-year experience. Plast Reconstr Surg. 2002;109(3):999-1006. doi:10.1097/00006534-200203000-00031.
- Shenaq SM, Klebuc MJ, Vargo D. Free-tissue transfer with the aid of loupe magnification: experience with 251 procedures. Plast Reconstr Surg. 1995;95(2):261-269. doi:10.1097%2f00006534-199502000-00005.
- Morrison WA, McCombe D. Digital replantation. Hand Clin. 2007;23(1):1-12. doi:10.1016/j.hcl.2006.12.001.
- Buncke HJ Jr, Schulz WP. Total ear reimplantation in the rabbit utilising microminiature vascular anastomoses. Br J Plast Surg. 1966;19(1):15-22. doi:10.1016/S0007-1226(66)80003-6.
Cite this article
Akelina Y. Microsurgical technique for 1mm vessel end to end anastomosis. J Med Insight. 2014;2014(2). doi:10.24296/jomi/2.