Laparoscopic Heller Myotomy
Main Text
Table of Contents
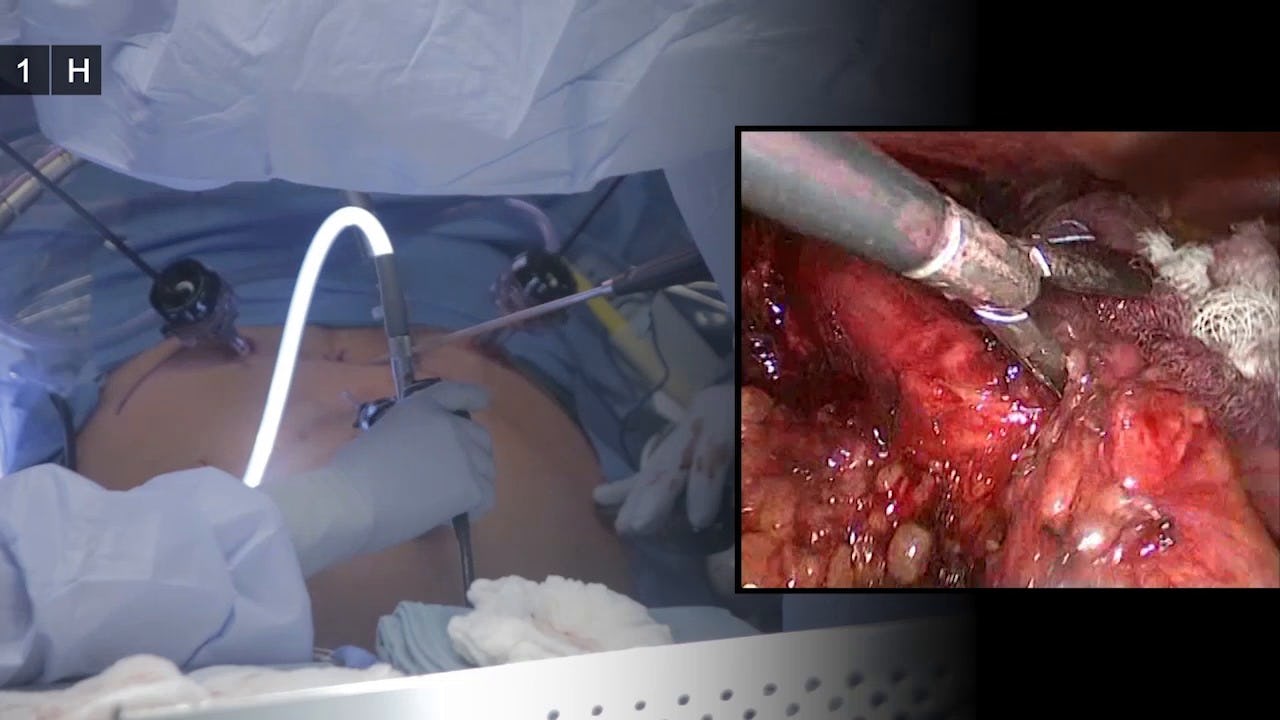
The gold standard for achalasia is surgical correction via laparoscopic Heller myotomy with a partial fundoplication. The goal of this technical report is to illustrate our preferred approach to patients with achalasia and to provide the reader with a detailed description of our operative technique, its rationale, and our pre and post-operative management.
Achalasia is a rare disorder of the esophagus, with an incidence of 0.5-1.2 in 100,000 cases/year, where the esophageal peristalsis is absent and the lower esophageal sphincter (LES) fails to relax, therefore causing dysphagia.1 This condition appears to be largely equally distributed among different races and gender groups. Some studies point to a bimodal age distribution, with peaks at 30 years of age and 60 years of age, while others indicated that the incidence of achalasia increases with age.
The most common presentation is dysphagia and regurgitation.2 Diagnosis is confirmed with barium esophagogram, upper endoscopy, and esophageal manometry. Manometry is the gold standard and usually shows failure of the LES to relax and complete loss of peristalsis. More refined diagnostics, such as the high resolution manometry (HRM), can identify variants and guide management based on predictable responses to medical and surgical treatments.5
Pneumatic balloon dilatation of the LES is a common approach to achalasia.6,7 However, there is a high rate of recurrence for which Heller myotomy with a partial fundoplication is a more definitive management. Newer techniques, such as the peroral endoscopic myotomy (POEM) are emerging but their performance as compared to the Heller myotomy is still to be determined.8,9
Heller myotomy (LHM) with Dor fundoplication is first line surgical treatment of achalasia. Mega-esophagus, defined as esophagus greater than 6 cm in diameter, is another esophageal pathology where studies have shown that LHM with Dor fundoplication provides excellent or good results in most of patients, even in those with a sigmoid shaped esophagus.3,1 0,11
The most common intraoperative complication of the Heller myotomy is an esophageal perforation. If the injury is recognized intraoperatively, then laparoscopic repair that includes closing the perforation with intracorporeal suturing using 4-0 absorbable sutures and a Dor fundoplication to patch the repair is sufficient. Risk factors for esophageal perforation are reoperation or previous botox injections. If an esophageal perforation is suspected immediately postoperatively, then a water-soluble contrast medium swallow is recommended and a covered stent placed with an upper endoscopy and broad antibiotic coverage is sufficient in most cases. For late presentation of esophageal perforation, an Ivor-Lewis esophagectomy is the treatment of choice as this operation will remove all the diseased distal esophagus.
Persistent or recurrent dysphagia may occur after a Heller myotomy. Persistent dysphagia may represent a technical problem with the myotomy or the fundoplication. Excessive narrowing of the esophagus can result from a short myotomy or a complete or near-complete fundoplication. Most of these cases can be corrected with pneumatic dilatation first, even though a wrong choice of fundoplication may warrant reoperation.
Recurrent dysphagia is defined as dysphagia that recurs after a period in which the patient has no symptoms. Recurrent dysphagia should raise concern for esophageal cancer, thus an upper endoscopy should be an essential part of the work up.13,14,15 If endoscopy rules out a malignancy, then one can offer the patient a pneumatic dilatation and a re-do Heller myotomy if this fails. 16,17,18 An esophagectomy is the last resort after failure of all other treatments.
Citations
- O'Neill OM, Johnston BT, Coleman HG. Achalasia: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2013;19(35):5806-5812. doi:10.3748/wjg.v19.i35.5806.
- Fisichella PM, Carter SR, Robles LY. Presentation, diagnosis, and treatment of oesophageal motility disorders. Dig Liver Dis. 2012;44(1):1-7. doi:10.1016/j.dld.2011.05.003.
- Willis T. Pharmaceutice rationalis sive diatribe de medicamentorum operationibus in humano corpore. London: Hagae-Comitis; 1674.
- Sadowski DC, Ackah F, Jiang B, Svenson LW. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil. 2010;22(9):e256-e261. doi:10.1111/j.1365-2982.2010.01511.x.
- Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 2008;135(5):1526-1533. doi:10.1053/j.gastro.2008.07.022.
- Sweet MP, Nipomnick I, Gasper WJ, et al. The outcome of laparoscopic Heller myotomy for achalasia is not influenced by the degree of esophageal dilatation. J Gastrointest Surg. 2008;12(1):159-165. doi:10.1007/s11605-007-0275-z.
- Weber CE, Davis CS, Kramer HJ, Gibbs JT, Robles L, Fisichella PM. Medium and long-term outcomes after pneumatic dilation or laparoscopic Heller myotomy for achalasia: a meta-analysis. Surg Laparosc Endosc Percutan Tech. 2012;22(4):289-296. doi:10.1097/SLE.0b013e31825a2478.
- Inoue H, Minami H, Kobayashi Y, et al. Perioral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42(4):265-271. doi:10.1055/s-0029-1244080.
- Ren Z, Zhong Y, Zhou P, et al. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc. 2012;26(11):3267-3272. doi:10.1007/s00464-012-2336-y.
- Liebermann-Meffert D, Allgöwer M, Schmid P, Blum AL. Muscular equivalent of the lower esophageal sphincter. Gastroenterology. 1979;76(1):31-38. doi:10.1016/S0016-5085(79)80124-9.