Flexor Digitorum Superficialis to Flexor Digitorum Profundus (STP) Transfer, Adductor Release, and Z-Plasty for a Pediatric, Stroke-Induced Left Hand Spastic Contracture
Main Text
Table of Contents
In this video, we demonstrate surgical correction of a severe hand deformity in a teenage girl with spastic hemiplegia. This patient has a non-functioning hand due to severe spasticity. Correction of the deformity is indicated primarily to facilitate hygiene and improve the position of the fingers. In some patients with volitional control, a certain degree of prehension may be achieved. The basic principles of deformity correction include differential sectioning of sublimis and profundus tendons followed by repair in a lengthened position. The first web contracture is released by muscular release and a skin Z-plasty.
This case involves an 11-year-old female who developed spastic hemiparesis following a bout of meningitis. Due to severe spasticity, she developed a flexion contracture of her fingers and an adduction contracture of the first webspace. She had little or no voluntary function in her hand. The finger deformity was so severe that her fingers were curled into her palm. This interfered with hygiene and she could not even cut her nails. The patient was also concerned about the appearance of her hand. Similar deformity can occur in adults with spastic hemiplegia following a stroke. The surgical procedure in children and adults is similar.
Most patients with such severe contracture have poor voluntary control of their hands. The goal of surgery is to improve finger and thumb position for hygiene and care. In patients with some voluntary muscle function, the improved position of the digits may lead to improved prehension. This patient had selective spastic hemiparesis that mainly involved her forearm and hand musculature and she had no cognitive involvement. Examination of the hand revealed a flexed position of the thumb at the interphalangeal joint and flexion of all fingers at the metacarpophalangeal (MCP), proximal interphalangeal (PIP), and distal interphalangeal (DIP) joints. The thumb webspace was contracted with an adduction deformity of the thumb metacarpal. The passive correction was very limited and extremely painful if attempted with force. Based on these findings we elected to proceed with a sublimis to profundus transfer, flexor pollicis longus lengthening, and release of the first webspace.
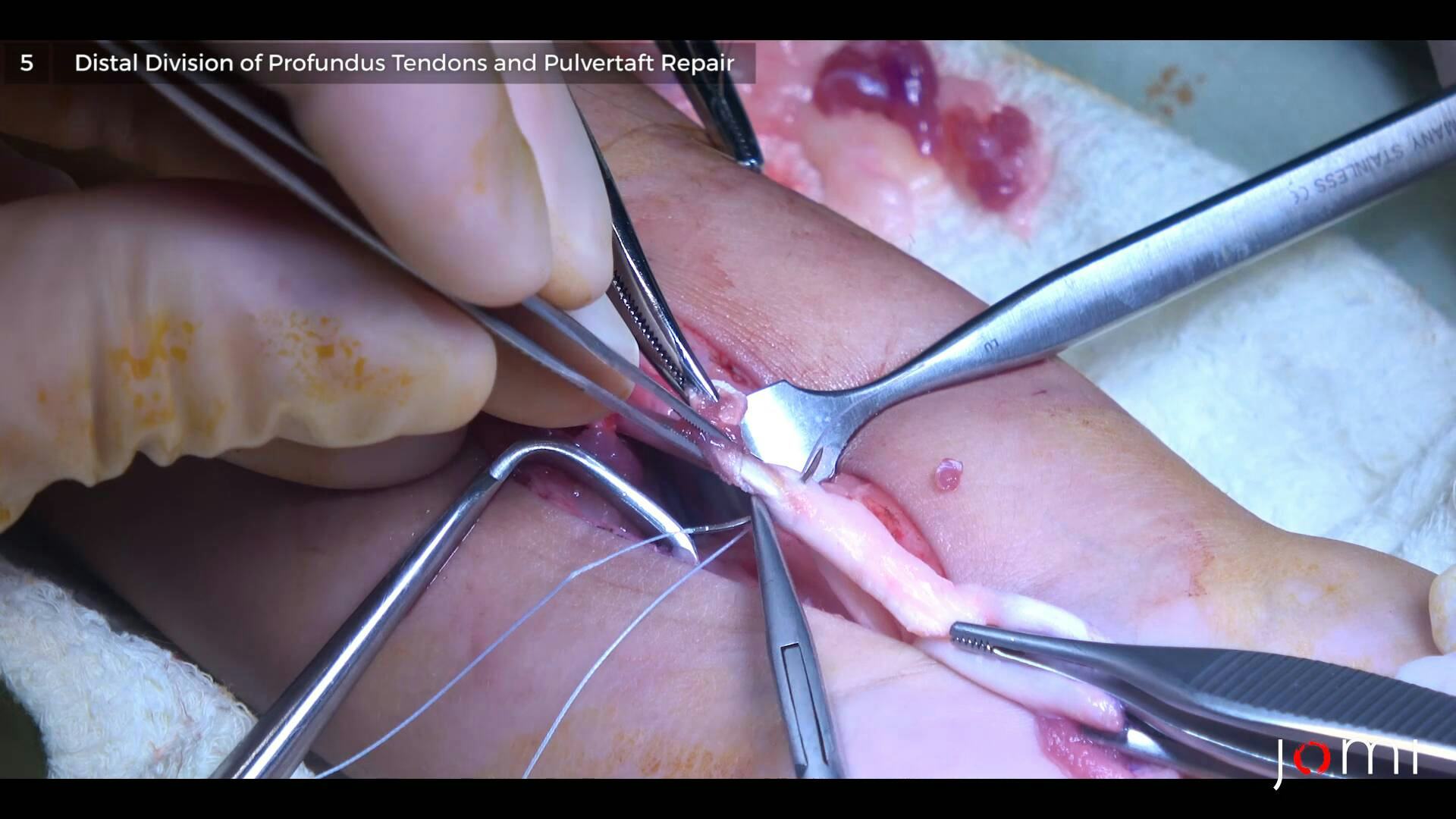
The procedure is performed under general anesthesia with tourniquet control. A longitudinal or gently curved incision is made in the distal forearm. Dissection is carried down through the deep fascia. It is important to identify and protect the median nerve and its palmar cutaneous branch throughout this procedure. The flexor pollicis longus, flexor sublimis, and flexor profundus tendons are identified. The flexor carpi radialis and flexor carpi ulnaris tendons, if contracted, can be lengthened by Z-plasty. The flexor pollicis longus tendon is addressed first. A long Z-lengthening is performed. The tendon ends are allowed to retract but not sutured at the present time. The individual sublimis tendons are identified and transected as distal as possible by flexing the fingers and wrist. The profundus tendons are now identified deep to the sublimis tendons. Individual tendons may not exist at this level and the entire mass of profundus tendons is transected as proximal as possible and by extending the fingers, the distal ends of these tendons slide towards the distal portion of the forearm. The wrist is held in neutral or 10 degrees of extension. The fingers are held in a gently flexed position at the MCP, PIP, and DIP joints, and without applying excessive tension to the proximal sublimis tendons, the proximal sublimis tendons are sutured to the distal profundus tendons in this functional position. It may or may not be possible to identify individual tendons. If possible, individual tendon repair can be performed. If not, the tendons could be repaired en masse. A Pulvertaft weave technique gives the strongest repair. We prefer using a combination of non-absorbable and absorbable 3/0 sutures of 3-0. With the wrist in a neutral position and the interphalangeal joint of the thumb in neutral extension, the flexor pollicis longus Z-plasty is repaired with interrupted 3-0 sutures. On completion of the tendon lengthening, the wrist and fingers should rest in a functional position.
The next part of the procedure involves correcting the thumb adduction contracture. If the thumb metacarpal is adducted and in the plane of the palm, then it effectively cannot be an opposable digit. The release of the thumb web space allows for improved appearance and the possibility of some grasp if the patient has a certain degree of voluntary muscle function. The degree of contracture can vary from mild to severe. Depending on the severity of contracture, the skin incision in the first web should be constructed as a 2- or 4-flap Z-plasty. Once the skin flaps are raised, careful deep dissection is performed and the first dorsal interosseous muscle and the adductor pollicis muscle are both identified. The adductor pollicis is divided just distal to its attachment on the third metacarpal. The first dorsal interosseous muscle is released from its origin on the thumb metacarpal and with passive abduction of the thumb metacarpal, a substantial degree of abduction is obtained. In cases of severe contracture, the trapezio- metacarpal joint capsule is released as well. Care should be taken to protect digital nerves to the thumb and index finger and the deep branch of the radial artery during deep palmar dissection. Prior to skin closure, it is important to release the tourniquet and achieve good hemostasis. After the reinflation of the tourniquet, the Z-plasty is repaired after flap transposition. Fine, absorbable sutures are used. Since many of these patients may not return for follow-up, the forearm incision is repaired in a similar manner. Release of tourniquet and hemostasis prior to definitive closure also avoids a potential risk of compartment syndrome should there be inadvertent bleeding. The hand is then immobilized in plaster splints, keeping the wrist neutral, fingers in a gently flexed position, and thumb in an abducted and opposed pos
ition. We prefer to leave the hand immobilized for three weeks, after which splints are discarded and the child is allowed to use his or her hand as tolerated. It may be prudent to use a brace intermittently especially in growing children to minimize the risk of recurrent contracture.
It is important to note for those in surgical training that sutures should be placed in a minimally invasive way; stitches with long tails and non-absorbable material can lead to excessive scar tissue with higher risk of adhesion of tendons and nerves.
Spastic disorders of the hand and upper extremity result from lesions of the brain and spinal cord. These include cerebrovascular accidents, anoxic brain injuries, trauma, and infections. Injury to the upper motor neuron (UMN) leads to weakness, incoordination, and spasticity in some or all muscle groups. In the early phase, the limb develops a positional deformity due to increased muscle tone and weakness of selective muscle groups. With time, a fixed contracture of varying degrees may result. In the hand, the usual deformity is one of wrist and finger flexion and thumb adduction. It is important to appreciate that this results from spasticity in both the extrinsic and intrinsic musculature. 1,2
Depending on the duration and severity of the neurological insult, the hand deformity varies in the degree of severity.3 At one end of the spectrum, the deformity is minimal, and the patient may have fair to good volitional control of the hand. Such patients benefit from therapy, bracing, selective muscle releases, and tendon transfer.
Severely affected patients have a non-functioning hand with marked flexion contracture of the wrist and fingers and adduction contracture of the thumb, termed thumb-in-palm (TIP) deformity. This may lead to skin maceration and problems with hygiene. Compressive neuropathy of the median nerve from a severe flexed position of the wrist is a known sequela and leads to unrecognized pain and increased spasticity.4
In such a severely deformed hand, bracing and therapy are often counterproductive, and surgery should be considered as part of a comprehensive care plan. Surgical treatment is generally delayed for at least a year following the neurological injury. Critical points in evaluating a spastic hand include assessing the degree of fixed and spastic deformity, the presence of spastic co-contraction of extrinsic flexor and extensor muscles,2 and the level of cognitive function or voluntary control, if any. It is important to assess the entire upper extremity and consider staged releases of the elbow and shoulder when indicated.
In a severely deformed, non-functional hand, one-stage comprehensive correction is achieved by lengthening or transecting the palmaris longus and flexor carpi radialis and ulnaris tendons, Z-lengthening of the flexor pollicis longus (FPL), superficialis to profundus (STP) transfer, and wrist arthrodesis with or without a proximal row carpectomy.1 Botte et al. described en-mass transection and repair of sublimis and profundus tendons.5 This technique is time-saving and does not affect the functional outcome. Lengthening of the extrinsic musculotendinous units will correct much of the deformity; however, flexion deformity is the result of spastic extrinsic and intrinsic muscles. If the intrinsic muscles are not addressed concurrently, the recurrent deformity is likely. Neurectomy of the motor branch of the ulnar nerve 6 and the recurrent motor branch of the median nerve 7 has been shown to improve the outcome and decrease the risk of recurrence. If there is residual metacarpophalangeal flexion contracture, then formal intrinsic release is performed through a dorsal incision on each finger. 1,7 A volar capsular release is indicated for severe contracture.
In cases of severe TIP deformity, lengthening of the FPL and neurectomy of the median motor branch will not suffice. Release of the thenar intrinsics including the adductor pollicis, flexor pollicis brevis, and first dorsal interosseous is necessary. 8 In addition, carpometacarpal (CMC) joint capsulotomy and first web Z-plasty may be necessary for adequate correction of the deformity.
As a result of this extensive one-stage correction, most patients will achieve satisfactory correction of the severe flexion contracture; thus, it results in facilitating hand hygiene and improving skin maceration and breakdown. Arthrodesis of the wrist in a functional position significantly decreases the potential for recurrent wrist deformity and obviates the need for long-term bracing. Complications following surgery include recurrent deformity, extension contracture from unrecognized extensor spasticity, and non-union of wrist arthrodesis.1
For our patient, we used a slightly different approach. Our patient was a teenager who had sustained a UMN lesion due to meningitis. The involvement was restricted to the wrist and hand. She had normal intelligence and good proximal voluntary control. She was concerned more about the appearance of the hand but also desired some function. Our surgical procedure was less radical and we did not perform ulnar and median neurectomies in an attempt to preserve any intrinsic function. Also, we achieved full wrist deformity correction and anticipated postoperative bracing to prevent recurrent deformity. We did not feel an arthrodesis was necessary, and the preservation of wrist motion was desirable in this situation.
We understand that there is potential for recurrent deformity and the need for future surgery. We took this limited surgical approach with the informed consent of the patient who understood the need for future procedures if indicated. Our goal was to preserve maximum function in this compromised hand and address future problems if and when they arise.
Citations
- Pomerance JF, Keenan MAE: Correction of Severe Spastic Flexion Contractures in the Nonfuntional Hand. J Hand Surg. 1996; 21 (A): 828-833. doi: 10.1016/S0363-5023(96)80199-7.
- Rhee CP. Surgical Management of Upper Extremity Deformity in Patients with Upper Motor Neuron Syndrome. J Hand Surg. 2019; 44 (A): 223-235. doi: 10.1016/j.jhsa.2018.07.019.
- Keenan MAE, Korchek JI, Botte MJ, Smith CW, Garland DE. Results of transfer of the flexor digitorum superficialis to the flexor digitorum profundus in adults with acquired spasticity of the hand. J Bone Joint Surg. 1987; 69 (A): 1127-1132. PMID: 3312205.
- Orcutt SA, Kramer WG III, Howard MW et al. Carpal tunnel syndrome secondary to wrist and finger spasticity. J Hand Surg.1990; 15 (A): 940-944. doi: 10.1016/0363-5023(90)90020-R.
- Botte MJ, Keenan MAE, Korchek JI. Modified technique for the superficialis-to-profundus transfer in the treatment of adults with clenched fist deformity. J Hand Surg. 1987, 12 (A): 639-640. doi: 10.1016/s0363-5023(87)80227-7.
- Keenan MAE, Todderud EP, Henderson R, Botte M. Management of Intrinsic Spasticty of the hand with phenol injection or neurectomy of the motor branch of the ulnar nerve. J Hand Surg. 1987; 12(A): 734-739. doi: 10.1016/s0363-5023(87)80059-x.
- Pappas N, Baldwin K, Keenan MAE: Efficacy of Median Nerve Recurrent Branch Neurectomy as an Adjunct to Ulnar Motor Nerve Neurectomy and Wrist Arthrodesis at the Time of Superficialis to Profundus Transfer in Prevention of Intrinsic Spastic Thumb-in-Palm Deformity. J Hand Surg. 2010; 35 (A): 1310-1316. doi: 10.1016/j.jhsa.2010.05.007.
- Matev I: Surgery of the spastic thumb-in-palm deformity. J Hand Surg. 1991; 16B: 703-708. doi: 10.1016/0266-7681(91)90160-P.