Right Open Indirect Inguinal Hernia Repair and Radical Inguinal Orchiectomy
Main Text
Table of Contents
An inguinal hernia is a condition where intra-abdominal organs bulge through the abdominal muscles or the inguinal canal. It is more common in males than in females and can occur at any age. Most adult inguinal hernias are considered acquired defects caused by weakness in the abdominal wall musculature due to excessive straining from heavy lifting, weight gain, coughing, or difficulty with bowel movements and urination. Inguinal hernias present as a bulge in the groin area that can become more prominent when coughing, straining, or standing up, and disappear when lying down. Symptoms are present in about 66% of affected people. Symptoms may include pain or discomfort, especially with coughing, exercise, or bowel movements. Medical history and physical examination are key to diagnosing inguinal hernias; however, imaging tests such as ultrasound, CT scan, or MRI can aid in the diagnosis when findings are equivocal. Inguinal hernias are generally classified as indirect, direct, or femoral based on the site of herniation relative to surrounding structures. In adults, watchful waiting is usually recommended for small and reducible inguinal hernias; however, inguinal hernias that enlarge, cause symptoms, or become incarcerated or strangulated are treated surgically. Surgical treatment can be divided into tissue repair and mesh repair with the latter being preferred due to having a lower recurrence rate.
An undescended testicle is a testicle that never moved to its proper position in the scrotum. The majority of these cases involve only one testicle, but around 10% can involve both. Complications involved with this condition include testicular cancer and infertility. Surgical correction is recommended before the child reaches 18 months old.
Here, we present a 78-year-old male who was diagnosed with a right inguinal hernia. Upon exploration, the right testicle was noted to be undescended and involved with the hernial sac. Based on the patient's age and the risk for future malignancy, the hernia repair also included an orchiectomy.
herniorrhaphy; indirect hernia; urology; surgery; mesh; undescended
Inguinal hernia (IH) repairs are among the most common surgeries performed each year. Estimates of the number of cases are around 20 million annually. Over 700,000 of those are performed in the US alone.1 IHs are much more common in males than females with a lifetime risk of 27% and 3%, respectively.2 Operative techniques involve both laparoscopic and open approaches. The advantages of the open approach include shorter surgical duration, less chance of serious complication, and a lower cost. The advantages of the laparoscopic approach include lower recurrence risk, less pain after the procedure, and quicker return to normal activities.3
This is the case of a 78-year-old male patient who presented with a bulge to the right inguinal area. Patients may present having recently noticed the defect or they may have known about the defect for a long time. In many cases, patients will not seek medical treatment until the IH either becomes larger or starts to cause pain or discomfort. Since a large number of IHs cause little to no discomfort, it is not uncommon for the patient to have had the defect for years before seeking a surgical correction.
Visualization and palpation of the affected area are staples of the physical exam for an IH. Hernias can be best evaluated with a hand placed in the groin and asking the patient to bear down (Valsalva) or cough. This maneuver will allow the physician to evaluate the size of the hernia as well as get a sense of how easily it can be reduced. Careful attention should also be paid to the skin overlying the hernia. Warmth, erythema, and edema are important observations. These can be especially concerning when the hernia is non-reducible as they are signs of bowel incarceration.
The diagnosis of IH is largely clinical. For the most part, a consistent patient history coupled with a physical exam is enough to diagnose an IH. In some cases, it becomes important to obtain more information about the exact location, size, or bowel integrity (potentially incarcerated hernias). CT, MRI, and ultrasound (US) are all modalities that are commonly used in the evaluation of IH. US provides the ability to obtain dynamic images by having the patient Valsalva during the study. It is generally the safest modality because it uses no radiation. However, images are extremely dependent on the technician’s experience and ability, and the patient’s body habitus.4 MRI is another viable modality but is used less often due to its expense and the extended time that it takes to obtain images. It has been demonstrated that MRI would be the imaging modality of choice in cases where occult IH is suspected and the physical exam is inconclusive.5 CT is also often used especially when there is a question of possible bowel incarceration. CT images are quick to obtain, and image quality is less affected by the experience of the technician. The limitation of CT is that images are typically obtained with patients in the supine position. This causes many IHs to reduce, thus making it more difficult to interpret the exact hernia type and location. There is some evidence to suggest that placing a patient in the prone position will use gravity to cause the hernia to protrude, thus giving the images more diagnostic detail.6
IHs almost always present as a noticeable bulge in the groin. Patients tend to notice these hernias more when squatting, straining (Valsalva), lifting, or performing other activities that increase intra-abdominal pressure. The size of hernia at presentation varies from patient to patient, as do the patient’s associated symptoms. Most commonly, a patient's presenting symptom would be pain associated with hernia protrusion either through the inguinal canal (indirect hernias) or through the abdominal wall (direct hernia). Pain occurs most commonly during periods of increased activity or rises in intra-abdominal pressure. Often, rest or lying down will cause the hernia to self-reduce and thus relieve the symptoms. Although hernias tend to be relatively benign defects, rarely they can incarcerate and cause life-threatening complications due to ischemic or necrotic bowel tissues.
For symptomatic patients, surgery remains the definitive treatment as it is extremely rare for a hernia to resolve on its own. Both laparoscopic and open repairs are used. IHs that are asymptomatic or do not cause unsatisfactory cosmetic appearance can be managed with a “watchful waiting” approach. Most of these hernias come out and then self-reduce with ease, and are thus not at significant risk for strangulation. In males, which account for the majority of IHs, the rate of incarceration with “watchful waiting” is <3%.7 Due to the low rate of strangulation, watchful waiting may be an appropriate option, especially if the patient is at increased risk of complications from surgery or anesthesia.
When the decision is made to operate on any kind of hernia, the goal is complete resolution of the defect. Mesh implantation tends to have slightly lower recurrence rates and thus is generally the preferred method.8 However, not every repair needs a mesh placement. If a primary tissue repair is a viable option, then suturing together the abdominal wall layers can provide enough strength to negate the need for a mesh implant. This decision is made on a case by case basis and is usually determined during the course of the surgery.
During the course of this patient’s IH repair, it was discovered that he had an undescended right testicle. While this is a fairly common occurrence in infants and children, it is rarely seen in adults. Studies have shown that an undescended testicle carries a slightly increased chance of developing testicular cancers.9 Given our patient's advanced age, it was decided to proceed with orchiectomy to mitigate this risk. It is worth noting here that this patient had consented for possible orchiectomy before the operation.
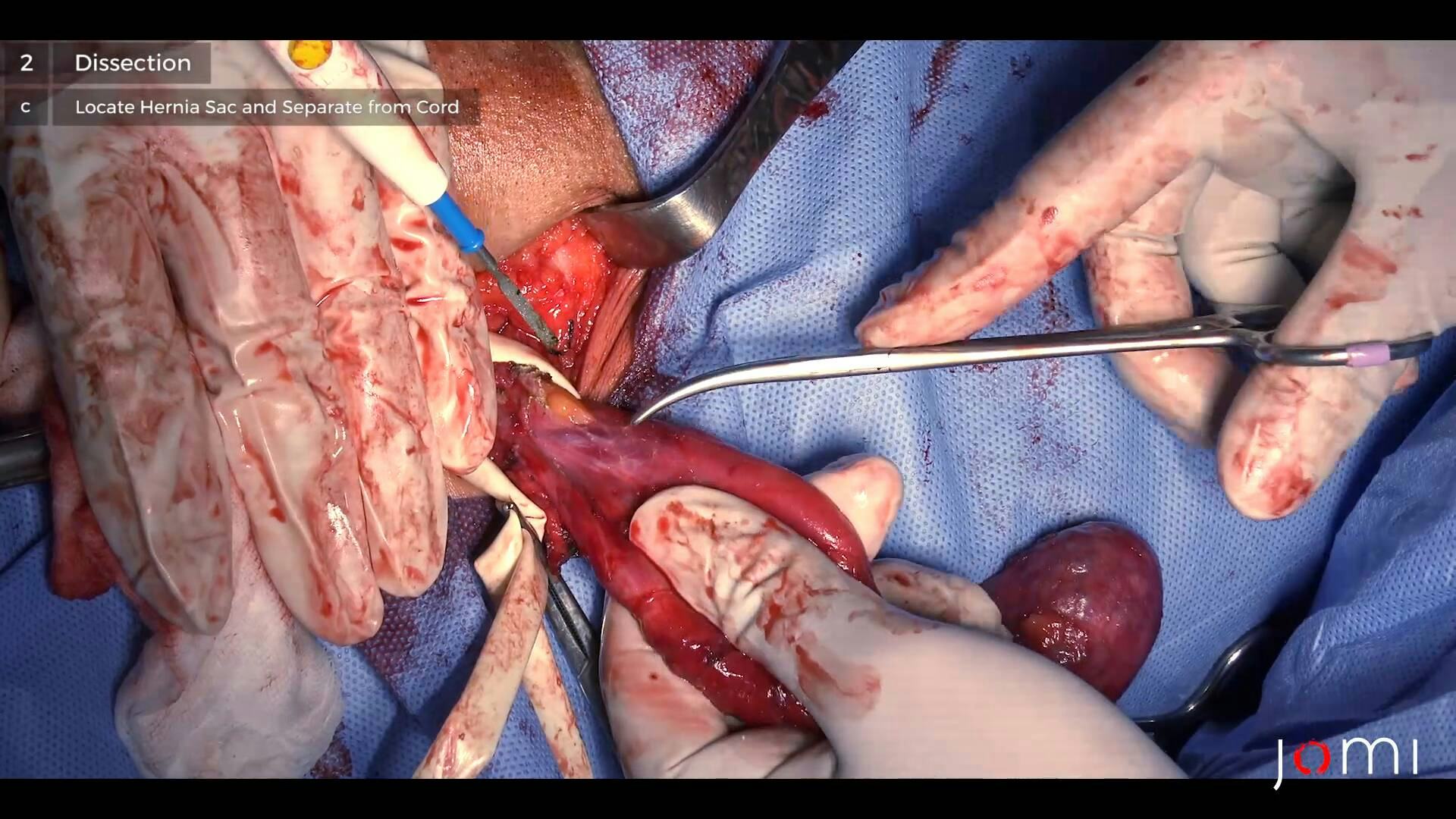
The patient who is presented in this case underwent a right-sided, open approach, indirect IH repair. In our patient’s case, he was also found to have an undescended testicle. Due to this anatomical defect, it was deemed necessary to perform a radical orchiectomy along with hernia repair. The original plan for the case was to repair the indirect hernia with mesh. However, the orchiectomy changed the course of the surgery. Instead of inserting mesh, the decision was made to perform a high ligation of the hernia sac and spermatic cord. Removing the spermatic cord allowed for complete closure of the deep inguinal ring and thus negated the need for a mesh implant.
Open IH repairs are carried out in stepwise fashion. To begin, a transverse incision is made in the groin crease, superior to the pubic tubercle. The incision is deepened until the spermatic cord can be visualized. Once the cord is visualized, the next step is to locate and dissect the hernia sac away from the spermatic cord. At this point in the operation, it becomes extremely important to preserve the structures of the spermatic cord as damage to its contents can lead to testicular ischemia and/or loss of fertility. As stated above, in this case, the spermatic cord contents were dissected out as part of the radical orchiectomy. Had this not been the case, a mesh implant would have been placed after ligation of the hernia sac. This would ensure that the contents would not be able to protrude back down through the inguinal ring. Once proper reduction and closure of the hernial defect are achieved, the layers of the abdominal wall are re-approximated. Once proper hemostasis is achieved, the site is then closed with subcutaneous sutures followed by skin closure.
After closure, the patient is taken to recovery. In the case of our patient, he will be started on a regular diet and if everything goes well, he will be discharged from the hospital the following day. Many patients can go home the same day. Age and comorbid conditions play a role in the decision to remain in the hospital for overnight observation. No strenuous exercise or heavy lifting is advised for 1–2 months postoperatively in order for complete healing to occur.
Hernia repairs are safe procedures with low 30-day mortality rates (0.1–3.2).1 The most common complication that can arise postoperatively is persistent pain in the groin. In most patients pain is mild, but up to 15% of patients report moderate to severe pain at one-year post-op or beyond.1,10 When compared with the laparoscopic approach, open repairs have a slightly higher chance of having this complication.
In general, the rates of hernia recurrence after a first-time operation range from 0.5–15%.8 This wide range is attributed to the various types of repairs as well as a wide range of surgeon experience. It is widely accepted that repairs done with mesh implantation have a lower recurrence risk than do non-mesh repairs. Likewise, it is accepted that laparoscopic repairs tend to have slightly fewer recurrence rates.1,8,11 Almost always, the presentation of recurrent hernias matches that of the first-time presentation. Operative techniques for recurrent IH are the same as for first-time repairs, and once again data shows that mesh implantation supersedes non-mesh repairs in lowering the risk of re-recurrent hernias.8
Open IHs require no special equipment outside of standard OR sets.
Nothing to disclose.
The patient referred to in this video article has given their informed consent to be filmed and is aware that information and images will be published online.
Citations
- Brooks D. Overview of treatment for inguinal and femoral hernia in adults. In: Post T, ED. UpToDate. Waltham, Mass.: UpToDate; 2020. www.uptodate.com. Accessed September 17, 2020.
- Vacca VM Jr. Inguinal hernia: A battle of the bulge. Nursing. 2017;47(8):28-35. doi:10.1097/01.NURSE.0000521020.84767.54.
- McCormack K, Scott N, Go PM, Ross SJ, Grant A. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database of Systemic Reviews 2003, Issue 1. Art. No.: CD001785. DOI: 10.1002/14651858.CD001785.
- Jamadar D, Jacobsen J, Morag Y,Girish G, Ebrahim F, Gest T, Franz M. Sonography of Inguinal Region Hernias. American Journal of Roentgenolgoy 2006. 187:1, 185-190. Doi:10.2214/AJR.05.1813.
- Miller J, Cho J, Michael MJ, Saouaf R, Towfigh S. Role of Imaging in the Diagnosis of Occult Hernias. JAMA Surg. 2014;149(10):1077–1080. doi:10.1001/jamasurg.2014.484.
- Miyaki, A., Yamaguchi, K., Kishibe, S. et al. Diagnosis of inguinal hernia by prone- vs. supine-position computed tomography. Hernia 21, 705–713 (2017). https://doi.org/10.1007/s10029-017-1640-9.
- Fitzgibbons RJ Jr, Ramanan B, Arya S, et al. Long term results of a randomized controlled trial of a non-operative strategy (watchful waiting) for med with minimally symptomatic inguinal hernias. Ann Surg. 2013;258(3):508-515.doi: 10.1097/SLA.0b013e3182a19725.
- Sarosi G, Ben-David K. Recurrent inguinal and Femoral Hernia. In: Post, T ED. UpToDate. Waltham, Mass.: UpToDate; 2020. www.uptoate.com. Accesses September 23, 2020.
- Michaelson D, Oh W. Epidemiology of and risk factors for testicular germ cell tumors. In: Post, T ED. UpToDate. Waltham, Mass.: UpToDate; 2020. www.uptodate.com. Accessed September 23, 2020.
- Bonwich J. Post-herniorrhaphy Groin Pain. In: Post, T ED. UpToDate. Waltham, Mass.: UpToDate; 2020. www.uptodate.com. Accesses September 23, 2020.
- Griffen F. Open surgical repair of inguinal and femoral hernia in adults. In: Post T, ED. UpToDate. Waltham, Mass.: UpToDate;2020. www.uptodate.com. Accessed September 23, 2020.